Peripheral Arterial Disease
Atherosclerosis
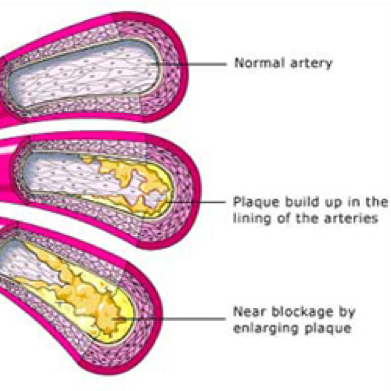
Peripheral Arterial Disease (PAD) is also known as atherosclerosis, poor circulation, or hardening of the arteries. Arteries are the blood vessels that carry oxygen and nutrient-rich blood from the heart to all areas of the body. Healthy arteries have a smooth lining that prevents blood from clotting and promotes steady blood flow. In PAD, the arteries slowly become narrowed or blocked when plaque gradually forms inside the artery walls. Plaque is made of excessive fat, cholesterol and other substances floating through the bloodstream, such as inflammatory cells, proteins and calcium. If the arteries become narrowed or blocked, blood cannot get through to nourish organs and other tissues, causing damage to the tissues and eventually tissue death.
The narrowing decreases the amount of oxygen getting to the calf muscles. This results in claudication.
Claudication is a term derived from the Latin word meaning “to limp”. Intermittent claudication (vascular claudication) describes the pain that develops in the muscles of the legs when taking exercise, such as walking. Commonly, the calf muscles are the most affected, and patients describe a cramping discomfort, as characteristic of the pain. Initially patients may be able to walk through the pain, but as the disease progresses further, this is not possible and the claudication pain causes limping and can only relieved by resting. Most patients find that their claudication symptoms are worse on walking uphill. Any situation in which the muscles of the legs have to work harder will worsen claudication symptoms. Some patients develop symptoms in their thighs and buttocks and PVD may also lead to impotence in men (Leriche syndrome). The development of particular claudication symptoms, depends on exactly which arteries are affected.The symptoms are intermittent because they resolve when resting.
In the later stages, arterial supply to the leg may be so poor that pain occurs in the toes and feet during periods of inactivity or rest. This is especially true at night. This is known as rest pain, which usually worsens when the legs are elevated and is often relieved by lowering the legs (due to the effects of gravity on the blood flow).
The most advanced stages of PAD can lead to Critical Limb Ischemia (CLI). Here the legs and feet have such severe blockages that they do not receive the oxygen rich blood required for growth and repair of painful sores and even gangrene (dead tissue). This condition, if left untreated, may require amputation.
Who is at risk?
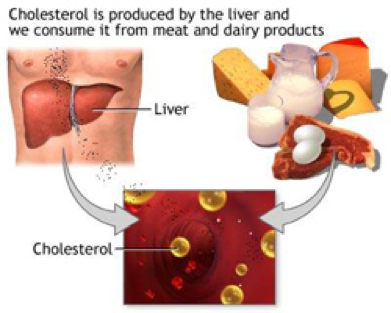
Cholesterol
An individual is at risk for developing PAD when one or more of these risk factors are present:
- Smoking
This is the number one risk factor for PAD. Those that smoke not only put themselves at risk for developing arterial disease but also undermine attempts at treatment. - Diabetes
Individuals with diabetes are at a higher risk for developing PAD - Age
Those 50 years or older are at greater risk to develop PAD. PAD affects both men and women, but occurs slightly more in men. The older you are the greater the risk of developing PAD - History of Heart Disease
If you or your family has a history of heart disease, you are at higher risk of developing PAD. - Hypertension (high blood pressure)
When blood pressure remains high, the lining of the artery walls becomes damaged. - Obesity
Being over weight increases the risk of peripheral vascular disease - High levels of Homocysteine
This is an amino acid found in plasma (blood). Some recent studies show higher levels are associated with PAD.
Diagnosis
The diagnosis is based on the history and examination and usually is followed by a duplex ultrasound. If more detailed information is needed or if intervention is being planned, an angiogram is usually requested. Also CT or MR angiograms can be very helpful.
Can PAD be treated?
Lifestyle changes including an exercise programme, medications and interventional procedures are the treatments available for PAD.
Initial treatment of PAD includes making lifestyle changes to reduce your risk factors. Changes you can make to manage your condition include:
· Quit smoking. Ask your doctor about smoking cessation programs available in your community.
· Eat a balanced diet that is high in fibre and low in cholesterol, fat and sodium. Limit fat to 30 percent of your total daily calories. Saturated fat should account for no more than 7 percent of your total calories. Avoid trans fats including products made with partially-hydrogenated and hydrogenated vegetable oils. If you are overweight, losing weight will help you lower your total cholesterol and raise your HDL (good) cholesterol. A registered dietician can help you make the right dietary changes.
· Exercise. Begin a regular exercise program, such as walking. Walking is very important and can aid the treatment of PAD. Patients who walk regularly can expect a marked improvement in the distance they are able to walk before experiencing leg pain. Ask your doctor if your hospital or clinic offers a structured, supervised walking program to help you succeed and maximize your exercise efforts.
· Manage other related health problems, such as high blood pressure, diabetes or high cholesterol.
· Practice good foot and skin care to prevent infection and reduce the risk of complications.
Foot Care Guidelines

Improving modifiable risk factors
- Every day, examine your legs as well as the tops and bottoms of your feet and the areas between your toes.
- Look for any blisters, cuts, cracks, scratches or other sores.
- Check for redness, increased warmth, ingrown toenails, corns and calluses. Use a mirror to view the leg or foot if necessary, or have a family member look at the area for you.
- Once or twice a day, apply a moisturizing cream or lotion to your legs and soles and top of your feet to prevent dry skin and cracking. Do not apply lotion between your toes or on areas where there is an open sore or cut. If the skin is extremely dry, use the moisturizing cream more often.
- Care for your toenails regularly. Cut your toenails after bathing, when they are soft. Cut toenails straight across and smooth with a nail file.
- If you have diabetes, it is important to see a podiatrist.
- Do not self-treat corns, calluses or other foot problems. Go to a podiatrist to treat these conditions.
- Don’t wait to treat a minor foot or skin problem. Follow your doctor’s guidelines.
Medications may be recommended to treat conditions such as high blood pressure (anti-hypertensive medications) or high cholesterol (statin medications). - An antiplatelet medication such as aspirin or clopidrogrel (Plavix or Iscover) may be prescribed to reduce the risk of heart attack and stroke.
- Cilostazol (Pletal) may be prescribed to improve walking distance. This medication has been shown to help people with intermittent claudication exercise longer before they develop leg pain and to walk longer before they must stop because of the pain. However, not all patients are eligible to take this medication. Your doctor will tell you if you are eligible.
Interventional procedures. More advanced PAD can be treated with interventional procedures such as angioplasty (to widen or clear the blocked vessel), angioplasty with stent placement (to support the cleared vessel and keep it open), or atherectomy (to remove the blockage).
In some cases, surgical procedures such as peripheral artery bypass surgery may be performed to reroute blood flow around the blood vessel blockage.
If any of these procedures are recommended, your health care team will give you more information about the procedures so you will know what to expect.
What are the conditions associated with PAD?
Patients with atherosclerosis affecting the legs (e.g. PAD) generally have atherosclerosis elsewhere, because atherosclerosis is a generalized disease. One can therefore develop serious health problems in other locations such as:
- Heart attack: if the disease has affected the arteries that supply the heart
- Stroke or TIA (Transient ischemic attack) : if the disease is in the arteries that supply the brain
- Renal artery disease or stenosis: a narrowing or blockage of the artery that supplies blood to the kidney
- Amputation: if the disease in the leg vessels is too advanced.
Can PAD be cured?
There is no “cure” for PAD. Quitting smoking, exercising regularly, limiting fat and following a healthy diet, and managing your risk factors—such as diabetes, high cholesterol and high blood pressure—can help to reduce the progression of the disease. The interventional options have limitations in what can be achieved.
Finally…
This website should have answered some of your questions, but remember that this is only a starting point for discussion about your treatment with the doctors looking after you.