Balloon angioplasty and stenting for obstructive venous lesions like May-Thurner
What is it?
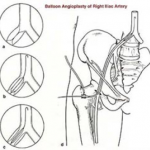
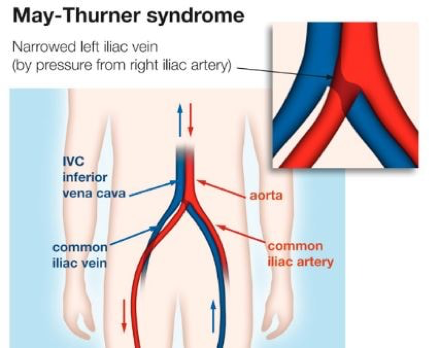 May-Thurner Syndrome (MTS) is a condition caused by the compression of the left common iliac vein by the right iliac artery leading to development of fibrosis (much like scar tissue) that results in narrowing of the vein. Different pelvic veins can be compressed at different points by segments of the artery or by overlying structures such as an enlarged uterus.
May-Thurner Syndrome (MTS) is a condition caused by the compression of the left common iliac vein by the right iliac artery leading to development of fibrosis (much like scar tissue) that results in narrowing of the vein. Different pelvic veins can be compressed at different points by segments of the artery or by overlying structures such as an enlarged uterus.
What are the common symptoms?
Some patients whose iliac veins are narrowed by 50% or more will develop some of the following symptoms including; leg pain (mostly after standing for an extended period of time or after exercise), swelling (oedema), pelvic pain, pain with intercourse (dyspareunia), pelvic pain after intercourse (post-coital pain), lower back pain, urinary bladder or bowel symptoms, bloating, leg veins, vulvar varicosities/varicocele or hemorrhoids.
What is the association with blood clots?
Some people who have a narrow iliac vein are more prone to developing thrombosis (clots) if they have additional risk factors for clotting such as being on oral contraceptives or estrogen therapy, pregnancy, extended periods of sitting or certain inherited disorders which increase the risk of abnormal clotting such as Factor V Leiden mutation, Factor II Prothrombin mutation, Protein S or Protein C deficiency or Anti-Thrombin III deficiency. This is known as iliofemoral deep vein thrombosis. Iliofemoral deep vein thrombosis usually presents with a sudden onset of leg pain, swelling and a blue discoloration of the leg. Roughly 80% of patients who develop iliofemoral deep vein thrombosis involving the iliac and leg veins will be found to have an iliac vein narrowing.
What are your treatment options?
When an iliac vein narrowing (stenosis) is discovered, this can be treated with placement of a stent in the vein. The stent is inserted into the compressed iliac vein by a needle stick approach in the groin. The stent usually yields impressive improvements in the quality of life for those who have severe symptoms from iliac vein compression.
Balloon Angioplasty & Stenting
How does a balloon angioplasty work?
Angioplasty and angioplasty with stenting are minimally invasive procedures performed to improve blood flow in the arteries or veins that are narrowed or blocked.
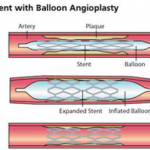
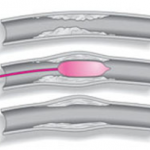
In the angioplasty procedure, imaging techniques are used to guide a balloon-tipped catheter, a long, thin plastic tube, into an artery and advance it to where the vessel is narrow or blocked. The balloon is then inflated to open the vessel, deflated and removed.
In vascular stenting, which is often performed with angioplasty, a small wire mesh tube called a stent is permanently placed in the newly opened artery to help it remain open. There are two types of stents: bare stents (wire mesh) and covered stents (with an additional artificial wall).
How do I prepare for an angioplasty?
You should report to your doctor all medications that you are taking, including herbal supplements, and if you have any allergies, especially to anaesthesia or to contrast materials also known as “dye” or “x-ray dye”). In most cases, you may take your usual medications, especially blood pressure medications. These may be taken with some water in the morning before your procedure.
You may be instructed not eat or drink anything for several hours before your procedure.
You may need to stay overnight at the hospital following your procedure.
You will be given a gown to wear during the procedure.
What does the equipment look like?
In these procedures, x-ray imaging equipment, guide wire, sheath, a balloon catheter and stent are used.
The equipment typically used for this examination consists of a radiographic table, an x-ray tube and a television-like monitor that is located in the examining room or in a nearby room. When used for viewing images in real time (called fluoroscopy), the image intensifier (which converts x-rays into a video image) is suspended over a table on which the patient lies
What actually happens during an angioplasty?
The exact technique may vary slightly but the general outline of the procedure is as follows. The procedure starts off in exactly the same way as an angiogram, and if you have already had this performed, you will know what to expect. You will lie on the x-ray table, generally flat on your back. You need to have a needle put into a vein in your arm, so that the anesthetist can give you a sedative or painkillers. Once in place, this will not cause any pain. You may also have a monitoring device attached to your chest and finger, and may be given oxygen through small tubes in your nose.
The Surgeon will wear a theatre gown and operating gloves. The skin near the point of insertion, probably the groin, will be cleaned with antiseptic, and then most of the rest of your body covered with sterile drapes.
The skin and deeper tissues over the entry vessel will be anaesthetized with local anesthetic, and then a needle will be inserted into the artery.
Once the surgeon is satisfied that this is correctly positioned, a guide wire is placed through the needle, and into the blood vessel.
Then the needle is withdrawn allowing the fine, plastic tube (catheter) to be placed over the wire and into the artery.
The surgeon will use the x-ray equipment to make sure that the catheter and the wire, are moved into the right position. Then the wire and the catheter will be moved so they pass into the narrowed area, and the Balloon is then inflated. This may need to be done several times in order for the narrowed area to open up sufficiently to improve the blood flow. Sometimes a stent will need to be inserted to keep the blood vessel open.
Will it hurt?
When the local anaesthetic is injected, it will sting to start with, but this soon wears off, and the skin and deeper tissues should then feel numb. After this, the procedure should not be painful. There will be a nurse and an anesthesist standing next to you and looking after you. If the procedure does become uncomfortable for you, then they will be able to arrange for you to have some painkillers through the needle in your arm. As the dye, or contrast medium, passes around your body, you may get a warm feeling, which some people can find a little unpleasant. However, this soon passes off and should not concern you.
How long will it take?
Every patient’s situation is different, and it is not always easy to predict how complex or how straightforward the procedure will be. Most angioplasties take about an hour, however this depends on the complexity of the situation and sometimes it might take several a little bit longer.
What happens afterwards?
You will be taken back to your ward on a trolley. Nurses on the ward will carry out routine observations, such as taking your pulse and blood pressure, to make sure that there are no problems. They will also look at the skin entry point to make sure there is no bleeding from it. You will generally stay in bed for a few hours, until you have recovered. You may be allowed home on the same day, or kept in hospital overnight.
What are the risks or complications?
Major complications following angioplasty are uncommon.
When angioplasty is performed, blockages can recur, although most of these vessels can be opened again successfully. You will need surveillance scans to protect the initial results.
- Pain or discomfort. This may require medication.
- Bleeding or bruising. This is usually reduced by applying pressure to the puncture site. This is more common if you are taking blood thinners such as Aspirin, Warfarin or Clopidogrel.
- A blood clot or excessive bleeding from the puncture site. This may require further treatment and/or corrective surgery.
- Infection. This could require antibiotics and further treatment.
- Damage to surrounding structures, requiring further treatment.
- An allergy to injected drugs may occur, requiring further treatment.
- Seizures and/or cardiac arrest due to anaesthetic toxicity.
- Faintness or dizziness, especially when you start to move around.
- The procedure may not be possible due to medical and/or technical reasons.
- The stent may suddenly close. This may require further treatment.
- The artery/vein can become narrowed or blocked again. This may require further treatment.
- Exposure to radiation whilst pregnant carries significant risk. You should avoid getting pregnant whilst being treated.
- An existing medical condition could worsen.
When angioplasty is performed, blockages can recur, although most of these vessels can be opened again successfully. You will need surveillance scans to protect the initial results.
Benefits
- Compared to surgical interventions such as bypass surgery, balloon angioplasty and stent placement are much less invasive and relatively low-risk.
- These procedures can be performed using local anesthesia and sedation.
- No surgical incision is needed—only a small nick in the skin that does not have to be stitched closed.
- You will be able to return to your normal activities shortly after the procedure.
Finally…
This website should have answered some of your questions, but remember that this is only a starting point for discussion about your treatment with the doctors looking after you. Make sure you are satisfied that you have received enough information about the procedure, before you sign the consent form.